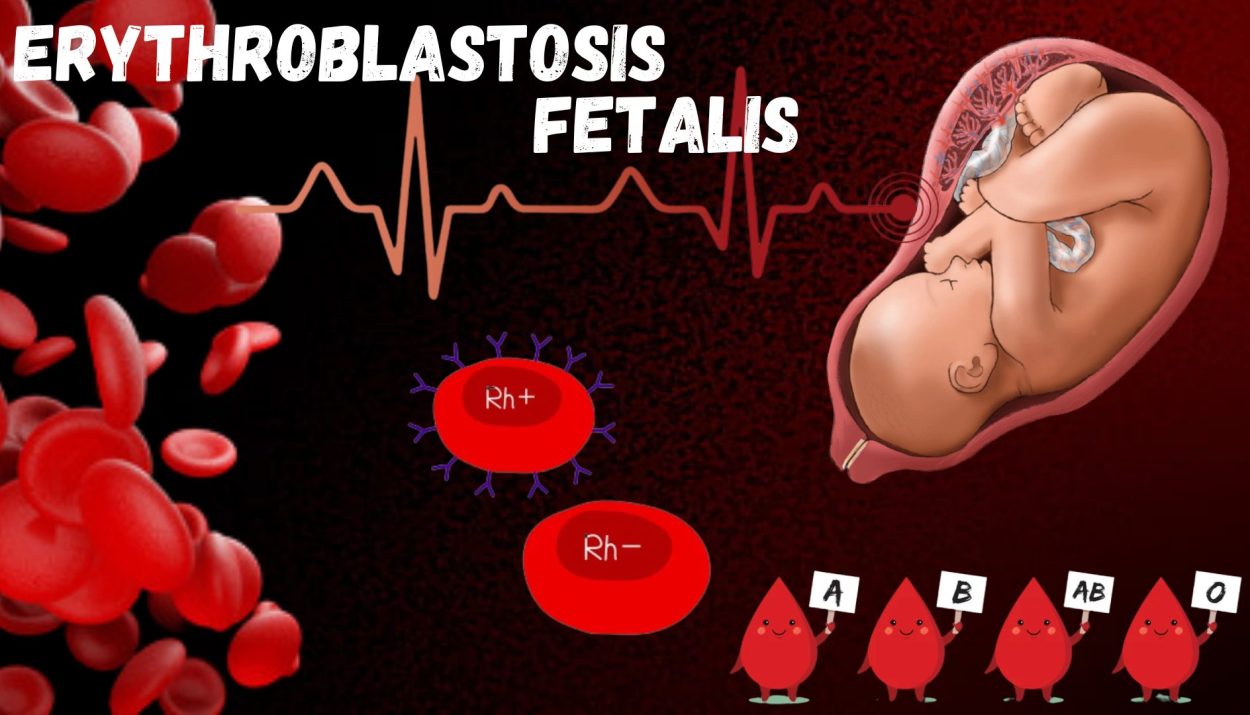
Erythroblastosis fetalis, also known as Hemolytic Disease of the Newborn (HDN), is a rare but potentially life-threatening blood disorder that affects newborns. This condition occurs when there is a mismatch between the blood types of the mother and the fetus, leading to fetal destruction as a result of an immune response triggered by the mother.
According to Merriam-Webster Dictionary–
“Erythroblastosis fetalis is defined as a hemolytic disease of the fetus and newborn that occurs when the immune system of an Rh-negative mother produces antibodies to an antigen in the blood of an Rh-positive fetus which crosses the placenta and destroys fetal erythrocytes and is characterized by an increase in circulating erythroblasts and by jaundice”.
Causes
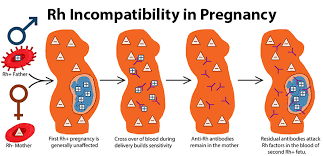
Erythroblastosis fetalis occurs when a pregnant woman’s blood type is incompatible with her developing baby’s. Rh incompatibility is responsible for complications in pregnancies. The condition commonly arises when a woman with Rh-negative blood (lacking the Rh factor) carries an Rh-positive baby. However, other blood type incompatibilities can also cause erythroblastosis fetalis, including ABO blood group incompatibilities.
The Rh factor is an inherited protein found on the surface of red blood cells. If a woman who lacks the Rh factor (Rh-negative) is sensitized to the Rh factor, her immune system may produce antibodies that attack the Rh-positive blood cells in her fetus. This immune response can lead to the destruction of fetal red blood cells and subsequent complications.
During pregnancy, the circulation of the fetus and the mother are distinct and separate from each other. However, certain antibodies from the mother, specifically of the immunoglobulin G (IgG) class, are capable of crossing the placenta and entering the fetal circulation. This allows the mother to pass on her immune protection to the developing fetus. While fetal red blood cells typically do not cross the placenta, there are tiny openings called microscopic pores through which a small number of fetal red blood cells can enter the mother’s circulation. When the placenta detaches from the uterine wall during delivery, a significant amount of fetal red blood cells can enter the mother’s circulation.
Let’s consider a scenario where the mother is Rh negative, meaning that Rh antigens are not present in her red blood cells. She is pregnant with her first child, who is Rh positive, inheriting the Rh antigen from the father. During this initial pregnancy with an Rh-positive fetus, the Rh-negative mother is generally not exposed to fetal red blood cells due to the separation of their blood circulations within the placenta. When the child is delivered, a significant amount of fetal red blood cells enters the mother’s circulation through microscopic pores in the placenta. These Rh-positive fetal red blood cells are perceived as foreign by the Rh-negative mother’s immune system, triggering the production of anti-Rh antibodies against the Rh antigen. Initially, these antibodies belong to the immunoglobulin M (IgM) class, which cannot cross the placenta and, therefore, do not pose a threat to the fetus.
Additionally, as the child is delivered, memory B cells specific to these Rh antigens are produced, indicating that the mother’s immune system has recognized the Rh antigen as non-self. This process is known as Sensitization. Sensitization of the mother’s immune system can occur earlier in the pregnancy, such as during prenatal bleeding, miscarriage, or medical termination of pregnancy. Now, let’s suppose the same Rh-negative mother becomes pregnant with a second Rh-positive child. Since her immune system has already been sensitized, memory B cells for Rh antigens are present. Some fetal red blood cells can enter the mother’s circulation through microscopic pores in the placenta. Once inside the mother’s circulation, these fetal red blood cells are sufficient to activate the Rh-specific memory B cells, resulting in the rapid production of anti-Rh antibodies. This time, these antibodies belong to the IgG class, which can cross the placenta and enter fetal circulation. These antibodies coat the fetal red blood cells and destroy them.
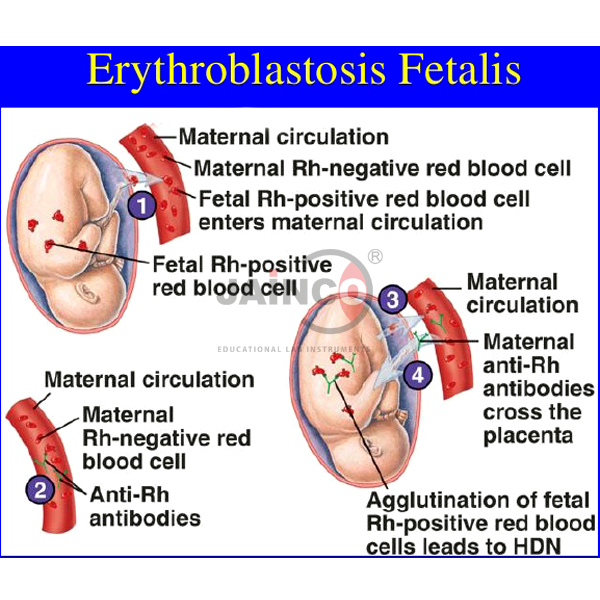
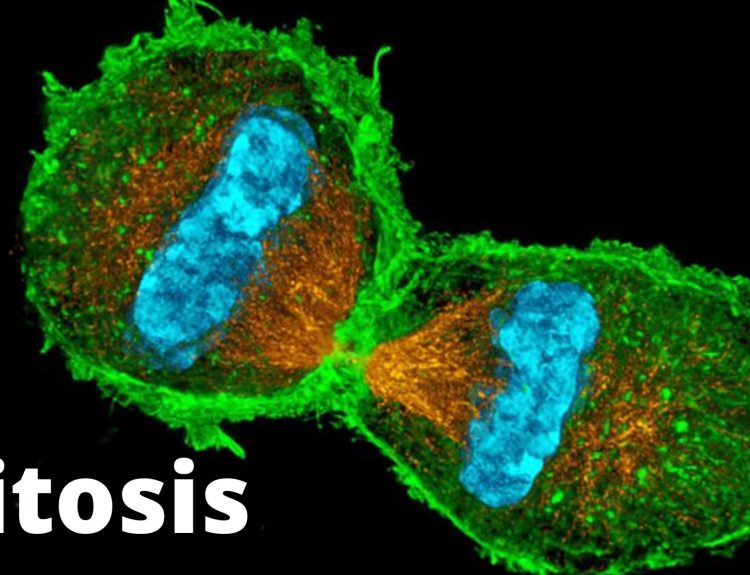
The destruction of fetal red blood cells, or hemolysis, leads to fetal anaemia. The severity of hemolysis determines whether the condition is mild, moderate, or severe. In cases of severe hemolysis, there is extensive and prolonged destruction of fetal red blood cells. To compensate for the loss, the liver, spleen, and other organs of the fetus increase their production of red blood cells, which results in the release of immature red blood cells, known as erythroblasts, into circulation.
Prevention
The prevention strategy for Erythroblastosis Fetalis involves a method called Passive Immunization. This approach aims to protect Rh-negative mothers from developing antibodies against the Rh factor and thus prevent complications in subsequent pregnancies.
To implement passive immunization, Rh-negative mothers are administered an anti-Rh antibody preparation commonly known as RhoGAM. The timing of administration is crucial for its effectiveness. During the first pregnancy, the Rh-negative mother is typically given the injection around 28 weeks of gestation. This timing ensures that if any mixing of blood occurs during childbirth, the anti-Rh antibodies are already present in the mother’s system, preventing sensitization.
Furthermore, after the delivery of the first child, a second dose of the anti-Rh antibodies is given to the Rh-negative mother within 24 to 72 hours. This postpartum administration helps eliminate any potential exposure to Rh-positive fetal blood that might have occurred during the delivery process.
By administering the anti-Rh antibodies at these specific time points, the passive immunization strategy aims to prevent sensitization of the Rh-negative mother’s immune system to the Rh antigen. This approach significantly reduces the risk of maternal antibody production against Rh-positive fetal red blood cells in subsequent pregnancies, thereby mitigating the development of erythroblastosis fetalis.
It’s important to note that this preventive measure does not eliminate the need for Rh immunoglobulin administration in subsequent pregnancies if the fetus is Rh-positive. However, by following the recommended administration schedule, the likelihood of sensitization and the associated complications of HDN can be greatly minimized.
References
erythroblastosis fetalis- Britannica
What is erythroblastosis fetalis?