Anti-microbial resistance (AMR) is a growing global concern that poses a significant threat to public health. It refers to the ability of microorganisms to resist the effects of antimicrobial drugs, rendering them ineffective in treating infections. The World Health Organization (WHO) has declared AMR as one of the top 10 global public health threats facing humans today. If left unchecked, AMR could lead to a future where common infections become untreatable, resulting in increased mortality rates and significant economic costs.
Microorganisms, which are living organisms that cannot be seen with the naked eye, are also referred to as microbes. These include bacteria, viruses, fungi, protozoa, and algae. Microorganisms are found everywhere on Earth, including in soil, water, and air, and in and on plants and animals. Some microorganisms can also cause diseases in plants, animals, and humans, while others are beneficial to our health, such as those found in our gut microbiome.
Understanding Anti-Microbial Resistance
Antimicrobial drugs are essential in treating bacterial, fungal, and viral infections. However, when these drugs are overused or misused, they can lead to the development of resistance in microorganisms. AMR occurs when bacteria, viruses, fungi, or parasites are no longer responsive to the drugs that were once effective in treating infections. This can lead to the emergence of “superbugs,” which are resistant to multiple drugs, making infections harder to treat.
Anti-microbial resistance (AMR) is a serious global health issue that threatens the effectiveness of antibiotics and other antimicrobial drugs in treating bacterial, fungal, and viral infections.
Causes of Anti-Microbial Resistance
AMR can occur naturally through the process of evolution, but it is also significantly influenced by human actions such as the overuse and misuse of antibiotics.
The overuse and misuse of antibiotics are major contributors to AMR. Antibiotics are frequently prescribed for viral infections, despite being ineffective against viruses, leading to the development of antibiotic-resistant strains of bacteria. In addition, antibiotics are widely used in livestock farming and aquaculture to promote growth and prevent diseases, leading to the spread of antibiotic-resistant bacteria in the environment.
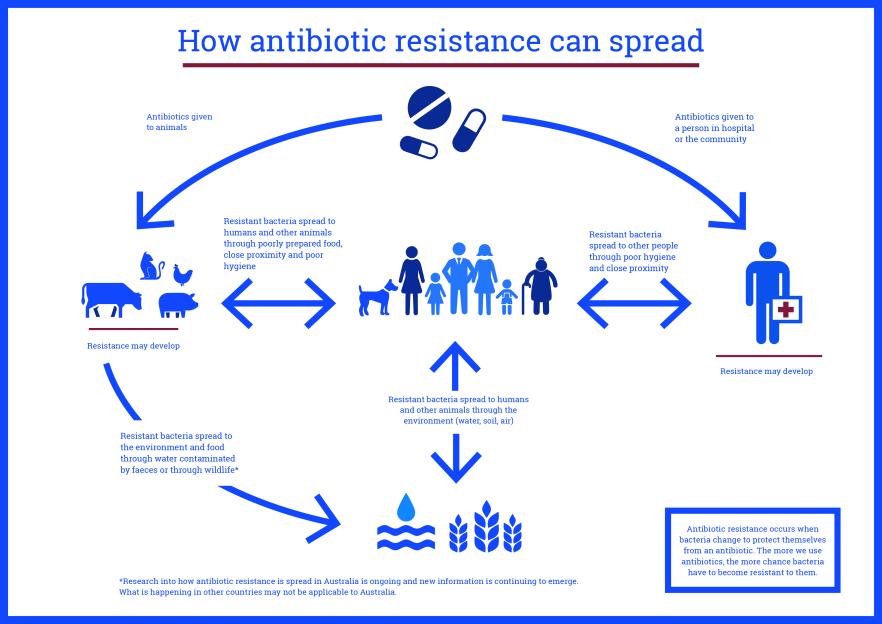
AMR can also be accelerated by poor infection control practices in healthcare settings and inadequate sanitation and hygiene. When healthcare providers do not follow proper infection control protocols, infections can spread rapidly, increasing the likelihood of AMR. Similarly, poor hygiene practices, such as not washing hands or improperly disposing of waste, can lead to the spread of bacteria and other microorganisms that can become resistant to antimicrobial drugs.
Consequences of Anti-Microbial Resistance
The consequences of AMR are far-reaching and potentially devastating. When antibiotics and other antimicrobial drugs become ineffective, the risk of infection increases and such infections can become more challenging to treat. This can lead to longer hospital stays, increased healthcare costs, and higher mortality rates. In some cases, conditions may be untreatable, resulting in significant public health risks.
The spread of superbugs can lead to the emergence of epidemics and pandemics, as seen with the recent COVID-19 pandemic. If antibiotic resistance continues to rise, we may face a future where we cannot rely on antibiotics to treat even the simplest of infections. AMR can also result in the loss of productivity, income, and increased poverty, particularly in developing countries where healthcare systems are under-resourced.
Possible Solutions and Preventive Measures
Addressing AMR requires a multi-sectoral approach involving governments, healthcare providers, the agriculture and food industry, and the public. Some possible solutions include reducing the overuse and misuse of antibiotics, promoting research and development of new drugs, improving infection control practices, and raising awareness among healthcare providers and the public. Preventive measures such as vaccination, good hygiene practices, and proper food safety practices can also help prevent infections and reduce the need for antibiotics.
Reducing the overuse and misuse of antibiotics is crucial in addressing AMR. Antibiotics should only be prescribed when they are necessary, and healthcare providers should follow proper prescribing guidelines. Antibiotics should not be prescribed for viral infections, as they are ineffective against viruses. The agriculture and food industry should also limit the use of antibiotics in livestock farming and aquaculture to prevent the spread of antibiotic-resistant bacteria.
Conclusion
The urgency of taking action is paramount when it comes to addressing the worldwide menace posed by AMR. It is essential to take steps to prevent the emergence and spread of AMR and to ensure the continued effectiveness of antimicrobial drugs in treating infections. This requires cooperation and coordination among various stakeholders and a concerted effort to raise awareness and implement effective measures. By addressing AMR, we can safeguard public health and ensure a sustainable future for generations to come.