Blood transfusion is a crucial medical procedure that involves transferring blood from one person (donor) to another (recipient) to restore blood volume, replace specific blood components, or improve overall health. However, not all blood types are compatible with each other and understanding blood types is essential to ensure a successful transfusion.
Blood consists of 55% Plasma containing antibodies, nutrients, salts and proteins, 1% are white blood cells and 44% of the blood is red blood cells.
The Basics of Blood Types
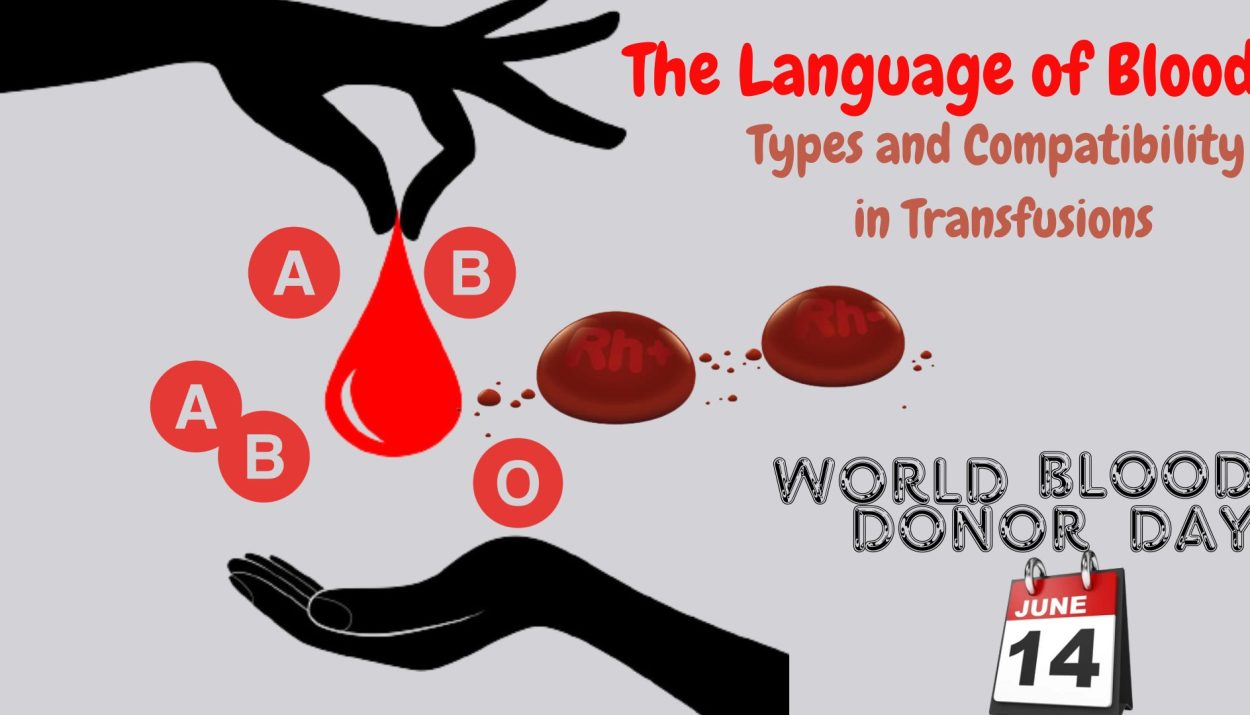
The ABO blood group system is one of the most well-known and widely used systems for categorizing human blood types. It classifies blood into four main types: A, B, AB, and O, based on the presence or absence of specific antigens on the surface of red blood cells (RBCs). These antigens are called A and B antigens.
Antigens are typically proteins or carbohydrates that are present on the surface of red blood cells (RBCs). They act as identification markers, distinguishing one individual’s cells from another’s. Antibodies, also known as immunoglobulins, are proteins produced by the immune system in response to the presence of foreign substances, such as bacteria, viruses, or incompatible blood types.
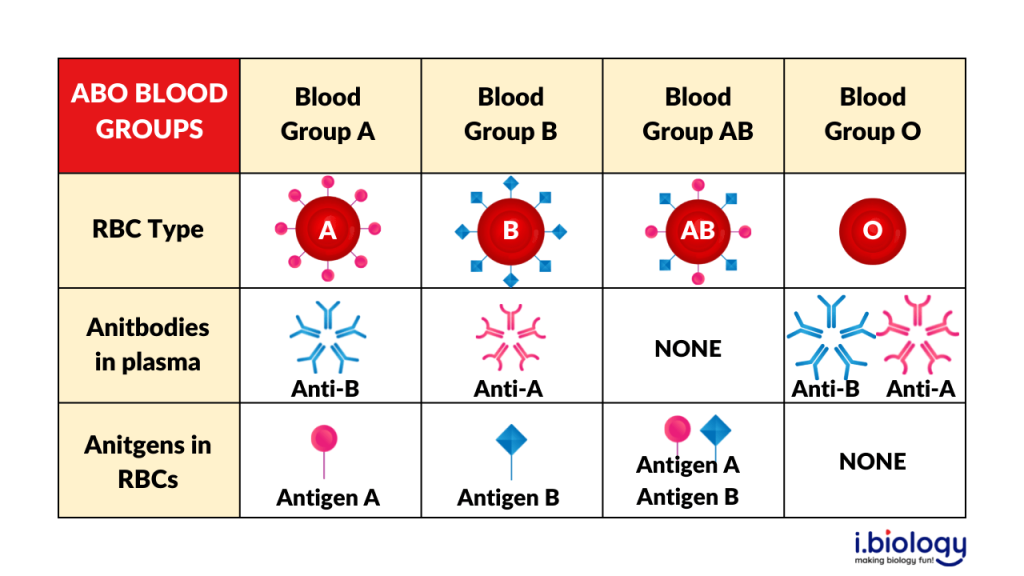
Blood Type A
Individuals with blood type A have A antigens on the surface of their red blood cells. Their plasma contains antibodies against the B antigen. Blood type A individuals can donate blood to those with blood types A and AB, while they can receive blood from individuals with blood types A and O.
Blood Type B
People with blood type B have B antigens on their red blood cells and antibodies against the A antigen in their plasma. Blood type B individuals can donate blood to those with blood types B and AB, while they can receive blood from individuals with blood types B and O.
Blood Type AB
Individuals with blood type AB have both A and B antigens on the surface of their red blood cells. They do not produce antibodies against either A or B antigens in their plasma. Blood type AB individuals are considered universal recipients because they can receive blood from any blood type (A, B, AB, and O), making them the most versatile blood type for transfusions. However, they can only donate blood to individuals with blood type AB.
Blood Type O
People with blood type O have neither A nor B antigens on the surface of their red blood cells. However, their plasma contains antibodies against both A and B antigens. Blood type O individuals are known as universal donors because their blood can be transfused to individuals with any blood type (A, B, AB, and O). However, they can only receive blood from individuals with blood type O.
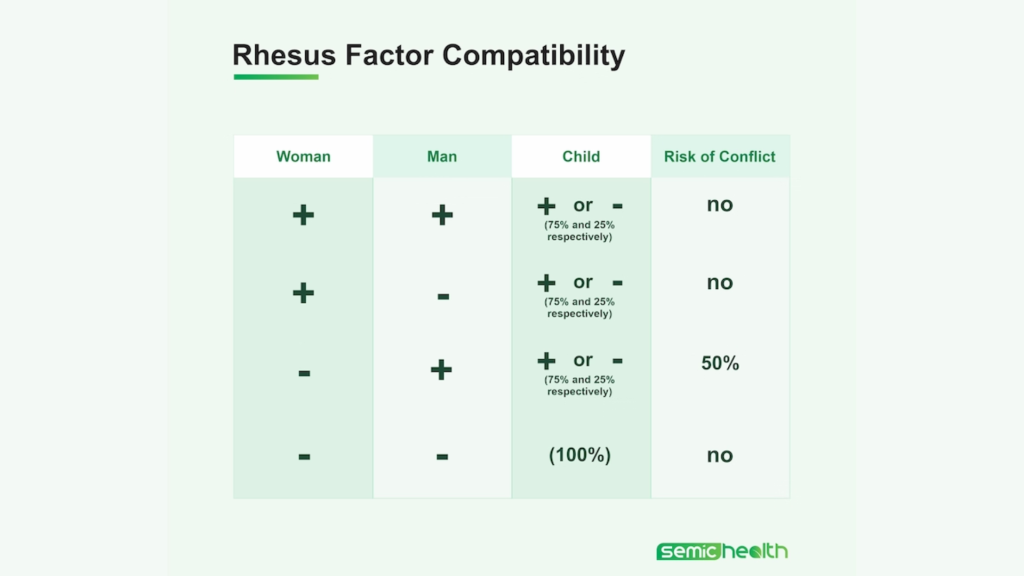
Rh factor
In addition to the A and B antigens, another crucial factor in blood typing is the Rh factor. This is a separate antigen that can be either present (Rh-positive) or absent (Rh-negative) on the surface of red blood cells. The ABO and Rh factors are combined to determine an individual’s complete blood type, such as A positive (A+), B negative (B-), AB positive (AB+), and so on.
Incompatibility between the blood types of a pregnant woman and her fetus related to the Rh factor results in Rh disease known as Erythroblastosis or hemolytic disease of the newborn (HDN). If an Rh-negative mother carries an Rh-positive fetus, her immune system may produce antibodies against the Rh antigen, considering it as a foreign substance.
Cross-Matching
Direct Antiglobulin Test (DAT)
The DAT, also known as the Coombs test, is performed to detect antibodies or complement proteins bound to the surface of red blood cells. The procedure involves taking a blood sample from the patient, washing the red blood cells to remove any unbound antibodies, and then adding an antibody reagent known as Coombs reagent to the washed cells. If the patient’s red blood cells are coated with antibodies, the Coombs reagent will bind to these antibodies, causing the cells to clump together (agglutination). Agglutination indicates a positive result, indicating the presence of antibodies on the patient’s red blood cells.
Indirect Antiglobulin Test (IAT)
The IAT also called the Indirect Coombs test, is used to detect antibodies in the plasma or serum that can cause the destruction of red blood cells. This test is commonly performed to determine the presence of antibodies in the recipient’s plasma that may react with donor red blood cells before a blood transfusion. In the IAT, a sample of the recipient’s plasma or serum is mixed with red blood cells of known antigens (typically from a blood donor). If there are any antibodies in the recipient’s plasma that are specific to the antigens present on the donor red blood cells, these antibodies will bind to the antigens, leading to agglutination.
Transfusion Alternatives
Autologous Transfusions
Autologous transfusion involves the process of collecting and storing an individual’s own blood prior to a planned medical procedure or surgery. The purpose is to have this stored blood available for transfusion during or after the procedure, reducing the need for allogeneic (donor) blood transfusions.
Directed Donations
Directed donations refer to blood donations made by individuals specifically for a particular patient. This approach is typically used when a patient has a rare blood type or requires repeated transfusions due to specific medical conditions. Directed donations can be made by family members, friends, or individuals with a close relationship with the patient.
World Blood Donor Day
The World Health Organization (WHO) designated June 14th as World Blood Donor Day to commemorate the birth anniversary of Karl Landsteiner, an Austrian biologist and physician who discovered the ABO blood group system, a groundbreaking achievement in the field of transfusion medicine.

The aim is to raise awareness about the importance of voluntary blood donation and to express gratitude to blood donors worldwide. This day serves as an opportunity to acknowledge the critical role of blood donors in saving lives and improving health outcomes for individuals in need.
The theme for the 2023 World Blood Donor Day campaign is “Give blood, give plasma, share life, share often” which emphasizes the role individuals play in supporting long-term transfusion needs and the importance of regular donations for a sustainable global supply of blood and plasma.
Conclusion
Understanding blood types and their compatibility is crucial in blood transfusions to ensure safe and effective procedures. The ABO blood group system and Rh factor play vital roles in determining compatibility, and proper matching is necessary to prevent adverse reactions. Cross-matching tests and alternative transfusion methods further enhance the safety and efficiency of blood transfusions. By adhering to these principles, healthcare professionals can minimize risks and maximize the benefits of this life-saving medical intervention.
References
World Blood Donor Donor Day– WHO
Autologous and Directed Donations